Q: Some surgeons are doing hair transplants using 5,000 to 6,000 grafts in a single surgery. Looking at the cases in your photo gallery, it seems like your hair transplants involve many fewer grafts per surgery. Do you do such large graft numbers in a single hair restoration procedure? — H.P., Cranston, R.I.
A: The goal in surgical hair restoration should be to achieve the best results using the least amount of donor hair (the patient’s permanent reserves) and not simply to transplant the most grafts in one session. In my opinion, although large sessions are very desirable, the recent obsession with extremely large numbers of grafts in one session is misplaced. The focus should be on results.
For example, I would prefer to have full growth with a properly placed 2,500 – 3,000 graft hair transplant session than partial growth in a 5,000 graft session. Of course, the 5,000 graft session will look fuller than 2,500 grafts but, in my experience, never twice as full, and never as full as two 2,500 graft sessions.
The ability to perform large sessions is possible because of the very small recipient sites needed in Follicular Unit Transplantation (FUT). It is one of the main reasons that we developed this procedure in back in 1995. See the first paper on this subject: Follicular Transplantation.
However, like all good things, the technique loses some of its advantage when taken to extreme.
In “very” large sessions, the long duration of surgery, the increased time the grafts are outside the body, the increased amount of scalp wounding, risk of poor growth, wider donor scars, placing grafts where they are not needed, sub-dividing follicular units, and the decreased ability to plan for future hair loss, can all contribute to suboptimal results. These problems don’t always occur, but the larger the session, the greater the risk. Therefore, it is important to decide if one’s goal is simply to transplant the maximum amount of hair that is possible in one session, or to get the best long-term results from your hair restoration.
Follicular Unit Preservation
One of the most fundamental issues is that doctors using very large sessions are not always performing “Follicular Unit Transplantation” and, therefore, in these situations the patients will not achieve the full benefit of the FUT procedure. Although doctors who perform these very large sessions take the liberty of calling their surgery “Follicular Unit Transplantation,” in actuality it is not, since naturally occurring follicular units are not always kept whole. The procedure is defined as follows: “Follicular Unit Transplantation is a method of hair restoration surgery where hair is transplanted exclusively in its naturally occurring, individual follicular units.” (see Hair Transplant Classification)
By preserving follicular units, FUT maximizes the cosmetic impact of the surgery by using the full complement of 1 to 4-hairs contained in naturally occurring follicular units. A whole follicular unit will obviously contain more hair than a partial one and will give the most fullness. Keeping follicular units whole also insures maximal growth since a divided follicular unit loses its protective sheath and risks being damaged in the dissection.
It can sound impressive to claim that you performing very large hair transplants, but if the large numbers of grafts are a result dividing up follicular units, then the patient is being short-changed. The reason is that, although the number of grafts is increased, the total number of hairs transplanted is not. A 3-hair follicular unit that is split up into a 1-hair and 2-hair micro-graft will double the graft count, but not change the total number of hairs actually transplanted. In fact, due to the increased dissection, more fragile grafts, and all the other potential problems associated with very long hair transplant sessions, the total number of hairs that actually grow may be a lot less. Please look at the section “Limits to Large Hair Transplant Sessions” on the Graft Numbers page of the Bernstein Medical – Center for Hair Restoration website for a more detailed explanation of how breaking up follicular units can affect graft counts.
Donor Scarring
Since there are around 90 follicular units per cm2 in the donor scalp, one needs a 1cm wide by 28cm long (11inch) incision to harvest 2,500 follicular units. A 5,000 follicular unit procedure, using this width, would need to be 22 inches long, but the maximum length one can harvest a strip in the average individual is 13 inches (the distance around the entire scalp from one temple to the other).
In order to harvest 5,000 grafts, one would need 5,000 / 90 FU/cm2 = 55.6cm2 of donor tissue. If one takes the full 13 inch strip (33cm), then it would need to be 1.85 cm wide (55.6cm2 / (33cm long) = 1.85cm wide) or 1.85/2.54= ¾ of an inch wide along its entire length. However, one must taper the ends of a strip this wide (you can’t suture closed a rectangle) and, in addition, you can’t take such a wide strip over the ears. When you do the math again, it turns out that for most of the incision, the width must be almost an inch wide, an incredibly large amount of tissue to be removed in one procedure.
This large incision obviously increases the risk of having a wide donor scar – probably the most undesirable complication of a hair transplant. Needless to say, very large graft counts are achieved by sub-dividing follicular units rather than exposing the patient to the risk of an excessively large donor incision.
Popping
There are other issues as well. Large sessions go hand-in-hand with very high graft densities, since you often need these densities to fit the grafts in a finite area. The closer grafts are placed together, the greater the degree of popping. Popping occurs when a graft that is placed in the skin causes an adjacent one to lift-up. When a graft pops (elevates above the surface of the skin) it tends to dry out and die. Some degree of popping is a normal part of most hair transplant procedures and can be easily controlled by a skilled surgical team, but when it is excessive it can pose a significant risk to graft survival.
The best way to decrease the risk of popping being a significant problem is to not push large sessions (and the associated very dense packing) to the limit. In a patient’s first hair restoration procedure, it is literally impossible to predict the likelihood of excessive popping and once a very large strip is harvested, or the recipient sites are created in a very large session, it may be too late to correct for this. In addition, popping can vary at different times during the procedure and in different parts of the scalp adding to the problem of anticipating its occurrence.
Even if the distribution of grafts is well planned from the outset, a very large first session may force the surgeon to place hair in less-than-optimal regions of the scalp when popping occurs. This is because the surgeon must distribute the grafts further apart and thus over a larger area to prevent popping.
Blood Flow
Particularly where there is long-standing hair loss, the blood flow to the scalp has decreased making the scalp unable to support a very large number of grafts. This is not the cause of the hair loss, but the result of a decreased need for blood when the follicles have disappeared. In addition, persons that have been bald for a long time often have more sun damage on their scalp, a second factor that significantly compromises the scalp’s blood supply and may compromise the follicles survival when too many grafts are placed in one session. As with popping, the extent of photo-damage, as seen when the scalp gets a dusky-purple color during the creating of recipient sites, often only becomes evident once the procedure is well under way.
In the healing process following the first hair transplant, much of the original blood supply returns and this makes the scalp able to support additional grafts (this is particularly true if one waits a minimum of 8-10 months between procedures). This is another reason why it is better to not to be too aggressive in a first session when there is long-standing baldness or significant photo damage and where the blood supply may be compromised.
Limited Donor Supply
Another issue that is overlooked in performing a very large first session is that the average person only has about 6,000 movable follicular units in the donor area. When 5,000 grafts are used for the 1st procedure there will be little left for subsequent sessions and limit the ability of the surgeon to increase density in areas such as the frontal forelock or transplant into new areas when there is additional hair loss.
Conclusion
There are many advantages of performing large hair transplants, including having a natural look after one procedure, minimizing the number of times the donor area is accessed, and accomplishing the patient’s goals as quickly as possible. However, one should be cautious not to achieve this at the expense of a wider donor scar, poor graft growth, or a compromised ability to plan for future hair loss.
Achieving very high graft numbers should never be accomplished by dividing up the naturally occurring follicular units into smaller groups, as this increases the risk to the grafts, extends the duration of surgery, increases the cost of the procedure (when charging by the graft) and results in an overall thinner look.
For further discussion see:
- The last section in Graft Numbers titled “Limits to Large Hair Transplant Sessions”
- Commentary: How large should hair transplant sessions be?


 Bernstein Medical – Center for Hair Restoration has moved to a new, state-of-the-art facility in mid-town Manhattan. The office is centrally located in the Park 55 building at 110 East 55th Street.
Bernstein Medical – Center for Hair Restoration has moved to a new, state-of-the-art facility in mid-town Manhattan. The office is centrally located in the Park 55 building at 110 East 55th Street.
 Follicular Unit Forum is unique in that it affords visitors an opportunity to anonymously ask questions about the “ins and outs” of hair transplant surgery, of those who actually have had the state-of-the-art Follicular Unit Hair Transplant procedures.
Follicular Unit Forum is unique in that it affords visitors an opportunity to anonymously ask questions about the “ins and outs” of hair transplant surgery, of those who actually have had the state-of-the-art Follicular Unit Hair Transplant procedures. “Dermatologic Clinics” is a quarterly review with comprehensive, state-of-the-art information by experts in the field of dermatology. The industries most highly knowledgeable medical professionals provide current, practical information on the diagnosis and treatment of conditions affecting the skin. Each issue of Dermatologic Clinics focuses on a single topic. The July 2005 issue, entitled “Advanced Cosmetic Surgery”, published an article authored by Robert M. Bernstein M.D, and co-authored by William R. Rassman M.D. entitled “
“Dermatologic Clinics” is a quarterly review with comprehensive, state-of-the-art information by experts in the field of dermatology. The industries most highly knowledgeable medical professionals provide current, practical information on the diagnosis and treatment of conditions affecting the skin. Each issue of Dermatologic Clinics focuses on a single topic. The July 2005 issue, entitled “Advanced Cosmetic Surgery”, published an article authored by Robert M. Bernstein M.D, and co-authored by William R. Rassman M.D. entitled “ Dr. Bernstein — and a Bernstein Medical – Center for Hair Restoration hair transplant patient — were featured on NBC television’s “Today” program with Matt Lauer. The segment, which mostly covered hair transplant repair procedures and hair restoration, was one of a three-part series on hair loss.
Dr. Bernstein — and a Bernstein Medical – Center for Hair Restoration hair transplant patient — were featured on NBC television’s “Today” program with Matt Lauer. The segment, which mostly covered hair transplant repair procedures and hair restoration, was one of a three-part series on hair loss. Surgery of the Skin: Procedural Dermatology; published in 2005 by Elsevier-Mosby and Edited by Robinson, Hanke, Sengelmann and Siegel; is monumental work that covers the entire spectrum of dermatologic surgical procedures. In the editor’s words, the goal of this 872 page textbook is:
Surgery of the Skin: Procedural Dermatology; published in 2005 by Elsevier-Mosby and Edited by Robinson, Hanke, Sengelmann and Siegel; is monumental work that covers the entire spectrum of dermatologic surgical procedures. In the editor’s words, the goal of this 872 page textbook is: “Hair Transplantation” is one in a series of medical textbooks published by Elsevier Saunders. The textbook — part of a series entitled Procedures in Cosmetic Dermatology — is written by Robert S Haber and Dowling B. Stough and edited by Jeffrey S. Dover. “Hair Transplantation” offers a step-by-step, practical guide to performing cutaneous surgical procedures.
“Hair Transplantation” is one in a series of medical textbooks published by Elsevier Saunders. The textbook — part of a series entitled Procedures in Cosmetic Dermatology — is written by Robert S Haber and Dowling B. Stough and edited by Jeffrey S. Dover. “Hair Transplantation” offers a step-by-step, practical guide to performing cutaneous surgical procedures. The Discovery Channel interviews Dr. Bernstein for a piece on
The Discovery Channel interviews Dr. Bernstein for a piece on  The
The  Dr. Bernstein received the 2001 HairSite.com award for excellence in hair transplantation. Here is the statement they made in giving Dr. Bernstein the annual award:
Dr. Bernstein received the 2001 HairSite.com award for excellence in hair transplantation. Here is the statement they made in giving Dr. Bernstein the annual award: New York — Follicular unit hair transplantation offers many advantages, but hair transplant surgeons continue to debate whether it is worth the effort.
New York — Follicular unit hair transplantation offers many advantages, but hair transplant surgeons continue to debate whether it is worth the effort.
 College of Physicians and Surgeons, New York.
College of Physicians and Surgeons, New York. The evolution of “follicular transplantation” can be attributed to three people. Dr. Robert Bernstein coined the phrase and advanced the concept. Dr. Bob Limmer ((Limmer B: Forum, Vol. 2, #2, 1991.)), ((Limmer B: J Dermatol Surg Oncol, 1994; 20:789-793.)) introduced the use of the binocular microscope, providing the technology, and Dr. David Seager showed by direct hair counts, comparing the growth of grafts cut with and without the microscope, how the hair growth was improved when the follicular unit was kept intact. ((4th Annual Meeting of the International Society of Hair Restoration Surgery September 19, 1996, “Does the size of the graft matter?”)), ((Seager, DJ: Micrograft size and subsequent survival — accepted for publication — Journal of Dermatologic Surgery.))
The evolution of “follicular transplantation” can be attributed to three people. Dr. Robert Bernstein coined the phrase and advanced the concept. Dr. Bob Limmer ((Limmer B: Forum, Vol. 2, #2, 1991.)), ((Limmer B: J Dermatol Surg Oncol, 1994; 20:789-793.)) introduced the use of the binocular microscope, providing the technology, and Dr. David Seager showed by direct hair counts, comparing the growth of grafts cut with and without the microscope, how the hair growth was improved when the follicular unit was kept intact. ((4th Annual Meeting of the International Society of Hair Restoration Surgery September 19, 1996, “Does the size of the graft matter?”)), ((Seager, DJ: Micrograft size and subsequent survival — accepted for publication — Journal of Dermatologic Surgery.))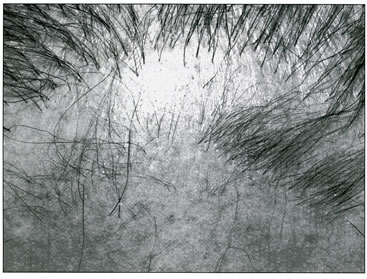

 I just returned from visiting Dr. Bob Bernstein in New York, and was impressed with his operation and even more impressed with his thoughts, observations, and insights into hair transplant surgery. He applies scientific methods to his work, is academically honest, and has an almost eerie instinctive knowledge of hair transplant surgery. Of course he has Dr. Bill Rassman to work with, but it is still remarkable. Dr. Bernstein is best known for introducing follicular transplantation ((R. Bernstein and W. Rassman Follicular Transplantation, International Journal of Aesthetic and Restoration Surgery. Vol. 3: No 2,1995, 119-132.)) to hair transplant surgery, an idea Bob Limmer has been pushing for ten years with the use of the binocular microscope, but no one would listen to him. Dr. Limmer, however, never used the term follicular transplantation. Using the microscope, you automatically dissect the follicular units. It can’t be avoided if done properly.
I just returned from visiting Dr. Bob Bernstein in New York, and was impressed with his operation and even more impressed with his thoughts, observations, and insights into hair transplant surgery. He applies scientific methods to his work, is academically honest, and has an almost eerie instinctive knowledge of hair transplant surgery. Of course he has Dr. Bill Rassman to work with, but it is still remarkable. Dr. Bernstein is best known for introducing follicular transplantation ((R. Bernstein and W. Rassman Follicular Transplantation, International Journal of Aesthetic and Restoration Surgery. Vol. 3: No 2,1995, 119-132.)) to hair transplant surgery, an idea Bob Limmer has been pushing for ten years with the use of the binocular microscope, but no one would listen to him. Dr. Limmer, however, never used the term follicular transplantation. Using the microscope, you automatically dissect the follicular units. It can’t be avoided if done properly.

 “Hair doesn’t grow singly it grows in naturally occurring groups of from one to four hairs. In follicular transplantation, we use these naturally occurring groups as the unit of the transplant,” he told CST.
“Hair doesn’t grow singly it grows in naturally occurring groups of from one to four hairs. In follicular transplantation, we use these naturally occurring groups as the unit of the transplant,” he told CST.




