Robert M. Bernstein, MD, New York, NY, [email protected]
The goals of most improvements in hair transplant techniques over the past 50 years have been to make donor harvesting less invasive, to increase accuracy for optimized growth, to generate grafts in a size that mimics nature, and to create recipient sites that result in natural hairlines that are aesthetically pleasing, but undetectable as a restoration.
One of the self-limiting factors in hair restoration, particularly follicular unit extraction (FUE), is that it has traditionally been subject to error caused by fatigue and other limitations of the human operator. This is a fundamental reason why the introduction of robotic technology for performing critical aspects of the FUE procedure has been such a game changer. In the hands of an experienced hair surgeon, the ARTAS™ Robotic Hair Transplant System is a powerful tool for creating natural and reproducible outcomes.
With the latest version of the platform, the recently released 9x upgrade, Restoration Robotics™ has engineered a faster and more accurate system for hair restoration. The improved accuracy of harvesting and shortened procedure increase graft viability. The smaller needles reduce scarring for a faster return to normal activity while allowing patients to wear shorter hairstyles.
Brief History of Hair Transplant Techniques
Norman Orentreich is widely credited with introducing the concept of “donor dominance” in the 1950s—the idea that transplanted hair continues to display the same characteristics of the hair from where it was taken. ((Orentreich N: Autografts in alopecias and other selected dermatological conditions. Annals of the New York Academy of Sciences 83:463-479, 1959.)) This means that continued growth at the recipient site is predicated on harvesting viable hairs from the donor site. In other words, the genetics for hair loss reside in the follicle rather than in the skin. However, due to limitations in graft harvesting technology, cosmetic outcomes of early transplant procedures were often unsatisfactory.
The large scars associated with early “hair plug” techniques were largely eliminated by the introduction of mini-grafts in the 1970s. ((Rassman WR, Pomerantz, MA. The art and science of minigrafting. Int J Aesthet Rest Surg 1993;1:27-36.)) This was followed by micro-grafts of 1-2 hairs. Mini-micrografting could be repeated hundreds or even thousands of times to cover large areas of baldness—but early manual techniques for doing so often yielded inconsistent graft quality and still resulted in scarring on the patient’s scalp, albeit less noticeable than previously. ((Rassman WR, Carson S. Micrografting in extensive quantities; The ideal hair restoration procedure. Dermatol Surg 1995; 21:306-311.))
In follicular unit transplantation (FUT), introduced in 1995 by Bernstein and Rassman, individual follicular units were dissected from the donor strip and became the new building blocks of the hair transplant. ((Bernstein RM, Rassman WR, Szaniawski W, Halperin A. Follicular Transplantation. Intl J Aesthetic Restorative Surgery 1995; 3: 119-32.)) Importantly, proper execution of FUT required the use of a stereo-microscope, a technique that was pioneered by Dr. Limmer. ((Limmer BL. Elliptical donor stereoscopically assisted micrografting as an approach to further refinement in hair transplantation. Dermatol Surg 1994; 20:789-793.)) FUT/strip became popular because it produced completely natural results with minimal recipient site scarring and could be used to cover large areas of the scalp.
A limitation of FUT, however, was that patients often needed to wear longer hair styles to cover the linear scar in the donor area. Nevertheless, FUT improved graft viability, consistency, and naturalness compared to mini-micrografting, and it remains in use today as an option for patients who want to maximize hair yield and are not concerned about the linear scar.
In the mid-1990s, Dr. Woods began using a small punch-like instrument to create small, circular incisions in the skin around follicular units, separating them from the surrounding tissue. The follicular units are then pulled, or extracted, from the scalp, leaving tiny holes that heal in a few days. Dr. Woods was reluctant to share his techniques with the medical community; in 2002 Drs. Rassman and Bernstein, working with Columbia University, developed their own technique and published it in Dermatologic Surgery. The procedure then spread rapidly, and now over half of all hair transplant procedures performed today worldwide utilize FUE techniques. ((Rassman WR, Bernstein RM, McClellan R, Jones R, et al. Follicular Unit Extraction: Minimally invasive surgery for hair transplantation. Dermatol Surg 2002; 28(8): 720-7.))
A major advance to the FUE technique came with the two-step process devised by Dr. Harris. In his technique, a sharp punch was first used to score the surface of the skin and then a dull punch was used to dissect deeper into the tissue to avoid transection of follicles. This two-step technique was to become the basis for the future mechanism of robotic FUE. ((Harris JA. The SAFE System: New Instrumentation and Methodology to Improve Follicular Unit Extraction (FUE). Hair Transplant Forum Intl. 2004; 14(5): 157, 163-4.))
FUE procedures allow recipients to wear shorter hairstyles due to the absence of a linear scar in the donor area, and they can typically return to physical activity sooner than after FUT. Yet, inherent difficulties in performing FUE, namely the requirement of keeping the follicular extraction instrument parallel and oriented along the axis of the follicle through the length of the graft, make it a technically challenging procedure. The introduction of the ARTAS Robotic Hair Transplant System in 2011 changed that dynamic by offering precision, control, and repeatability in follicle harvesting. Because it manages the exacting and repetitive work of extracting hundreds to thousands of grafts in a single session, physician fatigue and error are minimized. The potential to transect or damage the hair is reduced, and graft viability is increased.
Generational Improvements in Robotic Hair Transplantation
The first iteration of the ARTAS robot helped deliver accuracy and reproducibility in the form of a physician-assisted, computerized device with a three-dimensional optical system to locate and harvest follicular units directly from the donor area. By 2013, robotic recipient site making was added to help make the sites more uniform in depth and distribution and to avoid existing, healthy hair. Upon the recommendation of Dr. Bernstein, the manufacturer added another important upgrade in 2016 with a graft selection algorithm to select follicular units for harvesting based on the number of hairs they contain, producing greater hair density while leaving fewer scars in the donor area. ((Bernstein RM, Wolfeld MB. Robotic follicular unit graft selection. Dermatologic Surgery 2016; 42(6): 710-14.))
Restoration Robotics recently released the 9x ARTAS Robotic Hair Transplant System, the latest generation of its platform. It is faster and more accurate than previous versions and has better functionality. It also has improved artificial intelligence (AI) that reduces the potential for over-harvesting and enhances capabilities in recipient site making.
The easiest feature to appreciate with the 9x is that its raw speed is approximately 20% faster than the 8x. This is achieved by faster alignment with follicles, without sacrificing any precision in the approach angle for harvesting. The 9x features a dissection cycle of less than 2 seconds, meaning it can safely harvest roughly 1,300 grafts per hour—while still analyzing the scalp in micron-level precision. As with previous ARTAS versions, the cutting action is a two-step process, with an inner needle engaging the hair while the blunt outer punch separates the follicular unit from the remaining tissue.
Faster overall dissection is achieved with the 9x because the robot moves from one to the next follicle unit by skimming over the surface of the scalp, rather than retracting away from it between harvests.
The increased precision of the ARTAS 9x allows for the use of smaller needles for harvesting in appropriate candidates. The initial ARTAS system could only be used with a needle/punch apparatus that cut 1.0mm on the surface. The next iteration used a needle and punch of 0.9mm at the surface. The 9x has a 0.8mm option to allow very short hairstyles, although care should be taken in patient selection as there is less tolerance with a smaller punch.
The optics of the 9x have been completely reconfigured to use white LED illumination versus red, which allows extraction while harvesting without eye fatigue. The 9x is also easier to operate with some key features: a 1” extension on the robotic arm for longer reach and less need to reposition the patient; a smaller robotic head to permit acute angles of approach for harvesting; additional site making options, such as the ability to change the orientation (i.e., from sagittal to coronal) in different zones on the scalp; and a harvesting halo that is faster to apply and more comfortable for the patient.
AI and the Future of Hair Restoration
One of the more impressive aspects of working with the ARTAS System in hair restoration procedures is its already powerful AI. This feature makes it possible to detect select follicle units for harvesting. It also gives the platform the capability to automatically adjust the angle of approach, thereby reducing the potential to transect the hair follicle during harvesting.
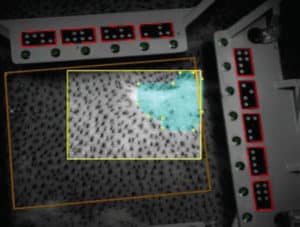
One of the major upgrades in the 9x is the addition of an “empty site warning” that signals the operator that the harvest is not precise, allowing for adjustments in real-time. This builds on the already intuitive and user-responsive interface to add further quality control. Automatic scar detection has also been added so that the robot will skip over low-density areas to have more uniform harvesting. This is particularly important to our practice where we specialize in repair and corrective procedures.
The ARTAS platform is integrated with ARTAS Hair Studio™, an app-based technology with which the surgeon can consult with the candidate to simulate the final outcome. The ARTAS Hair Studio is also used by the physician to design the pattern for recipient site creation. With the 9x, Hair Studio has been upgraded so that instead of stitching together multiple photos to create a three-dimensional representation of patient’s scalp, it does so in a single photograph, making it faster and more efficient.
What is fundamental to understand about the 9x upgrade is that many of the additions have been specifically engineered based on user feedback, my own included. Restoration Robotics continues to work closely with physician users to understand needs in the clinic to produce a platform for hair restoration that is responsive to needs of the end user and the end beneficiary (the patient). In my hands, the 9x takes and makes an already powerful tool for hair restoration even faster and more accurate.
The statements, views, opinions, and analysis concerning Restoration Robotics and its technology expressed in this article are solely mine and are not intended to reflect the statements, view, opinions, and analysis of Restoration Robotics.
Posted by