Robert M. Bernstein, MD, New York, NY, rbernstein@bernsteinmedical.com; Michael B. Wolfeld, MD, New York, NY, mwolfeld@bernsteinmedical.com; Jennifer Krejci MD, San Antonio, TX, jkrejci@limmerhtc.com
Disclosures: Dr. Bernstein and Dr. Wolfeld hold equity interest in Restoration Robotics, Inc. Dr. Bernstein is a medical consultant to the company and is on its medical advisory board.
ABSTRACT
Since the introduction of robotic FUE technology over five years ago, there have been numerous upgrades to the system. The current paper describes the most recent advances. These include a more user-friendly interface, the ability to select for larger follicular units, greater range-of-motion of the robotic arm, improved methods for stabilizing the scalp and newly designed needles for more accurate harvesting.
Background
The ARTAS Robotic System, developed by Restoration Robotics Inc., was first available for commercial use in 2011. Continued improvements in both its hardware and software have made it an increasingly valuable tool for physicians performing follicular unit extraction (FUE). Over 180 hair restoration surgeons world-wide currently use robotic technology to assist them in their FUE procedures. Recent advances in the robotic system have increased its speed and precision and new modifications have made it more user-friendly. The robotic system can be used for both harvesting and site creation. This writing focuses on improvements to robotic graft harvesting.
Touchscreen User Interface
The robotic system is an interactive, computer-assisted suite of hardware and software that uses optical-guidance robotics to identify and isolate follicular units in the donor area and create sites for grafts in the recipient area. In the earlier iterations, doctors used a mouse to control the operations of the robot. This required the physician to be seated with one hand resting on the mouse and slowed down the procedure. A touch screen has been developed to make operating the robot more intuitive and to speed up the ability to make real-time adjustments while the physician is standing and observing the patient. Most of the controls are aggregated to one area on this screen for ease of use. The touchscreen can be used alone or with the traditional mouse and keyboard, depending upon the user’s preference. (Figure 1.)
Follicular Unit Graft Selection
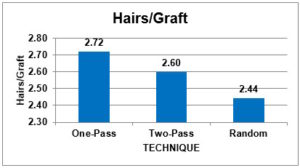
The follicular unit (FU) graft selection capability of the robotic system has been added to enable physicians to select follicular units based on hair content. The physician now has the option to harvest larger follicular units and skip over smaller ones, particularly one-hair units. The purpose is to harvest the most hair through the smallest number of wounds. FU graft selection has two main benefits: 1) It can generate a greater number of larger FU grafts to maximize the fullness of the restoration, and 2) it can be used to harvest larger FUs that can be microscopically dissected to generate a greater number of smaller grafts with a minimal number of donor wounds. Skipping over one-hair follicular units increases the number of hairs per graft by 11.4% with the one-pass method (selecting for FUs with 2 or more hairs) and 6.6% with the two-pass technique (adding a second pass to harvest 1-hair FUs skipped in the first pass) compared to a random selection of grafts. ((Bernstein RM, Wolfeld MB. Robotic follicular unit graft selection. Dermatologic Surgery 2016; 42(6): 710-14.)) (Figure 2.)
Locking Tensioner Tool
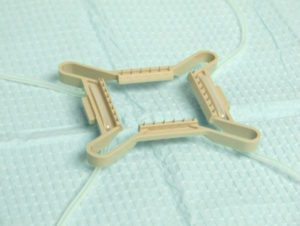
The tensioner is a compressible, polycarbonate device that is used to assist the vision system and to stretch and stabilize the skin prior to extraction. Fiducials, on the top of the tensioner’s rectangular surface, are used by the robot’s optical system to orient the arm for harvesting and to record the location of previously harvested grafts. (A fiducial is a marker placed in the field of view of an imaging system for use as a point of reference or a measure.) The undersurface has pins that grip the skin. (Figure 3.) The tensioner is compressed with a handle placed on the donor scalp and then allowed to passively expand, stretching the skin. (Figure 4.) It is secured with elastic straps to the patient’s headrest. (Figure 5.)
The re-designed tensioner tool has a thumb-activated catch and release mechanism, so that once the tensioner is grasped, constant pressure is not needed. This makes it easier to operate and places significantly less stress on the physician’s hands. It also allows the tensioner and handle to be loaded and placed on a stand that holds the instrument and protects the pins when not in use. This keeps the handle in a position to be grabbed easily. (Figure 4.) The handle can thus be set up in advance, increasing the speed of this step of the procedure.
Improved Halo
The tensioner is held in place by 1) pins that grip the skin, 2) the recoil of the compressed tensioner, and 3) elastic straps that are stretched and secured in grooves located on the base of the headrest and/or on a halo device. The advantage of a halo is that the forces are lateral (rather than downward) and thus more comfortable for the patient. It also causes less torque on the tensioner, allowing it to better follow the contour of the patient’s scalp. A newly designed halo has a double-notch and central protuberance that makes the bands more secure and enables the physician to more rapidly secure the bands using one hand. (Figure 5.)
Arm Spacer to Increase Range of Motion
A one-inch extension of the robotic arm allows the instrument to harvest at a more acute angle than was previously possible. It also increases the range of motion of the robotic arm. It is particularly useful when harvesting on the sides and lower occipital regions of the scalp. The greater reach increases the number of grafts that can be harvested without repositioning the patient, thereby saving operating time and leaving the patient undisturbed. (Figure 6.)
Improved Image Processing for Glare
Glare can interfere with the optimal functioning of the optical system. It may be caused by the light of the needle mechanism or the natural light of a bright operating room. When glare is present, it affects how the system identifies the hair and can prevent the system from recognizing hair that would be eligible for harvesting. With improved digital image processing, the system can better visualize existing hair, even in areas of glare within the grid. As a result, the number of grafts harvested per grid is increased.
Assisted Force-Drag
For the robotic arm to engage with the donor scalp, it must be aligned with the fiducials on the top of the tensioner. In the past, this alignment had to be performed manually. The new “Assisted Force-Drag” technology enables the robot to self-align to the tensioner as soon as the fiducials are detected by the vision system. This feature obviates the need for the manual step and allows for an overall faster workflow.
Puncture Depth (PD) Band Detection
The robot uses a two-step, sharp/blunt punch technique based on the ideas of Dr. Jim Harris. Puncture depth bands enable the robot’s computer to measure the depth of the needle (punch) in the scalp. The robot then uses this information to improve the accuracy of the subsequent puncture. Puncture depth band detection may be affected by the presence of blood, hair, and shadows from the tensioner. Improved algorithms that guide PD band detection have increased its accuracy by 9% compared to earlier versions, even in the face of these artifacts. (Figure 7.)
4-Prong Needle
The robot was initially designed with a two-pronged, sharp-punch. The advantage of this design was that the long prongs were able to anchor lax skin. A disadvantage was that it was less efficient when the scalp was tighter, or more fibrotic, and when the arm had to operate at a more acute angle to the surface of the scalp. To mitigate this limitation, a 4-prong needle was developed. The 4-prongs allow for cleaner incisions with better anchoring to tissue at acute angles. This advance results in improved yield, especially in areas below the occiput and on the side of the head. It is also more effective in patients with tougher tissue. (Figure 7.) A 3-pronged needle is currently being developed for tight and/or fibrotic skin as well as lax skin.
6-mm Punch
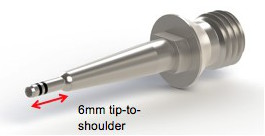
The original robotic system used a 4-mm rotating dull-punch to dissect the body of the graft from the surrounding tissue. The limitation of this design is that it was less effective in patients with longer hair follicles (i.e., greater than 4.5mm). With longer hair follicles, the collar of the 4-mm punch pushed on the skin and, as a result, splayed the grafts and/or bent the bulbs.
The new punch is 6-mm tip-to-shoulder so that full dissection of longer follicles can be accomplished with less distortion of the skin. This modification avoids damage to the lower portion of the grafts. (Figures 8, 9.).
The Future
A host of new modifications are in the pipeline. In addition to the 3-prong needle, a color camera is being developed that allows the robot to read white-light. This will make the operating field easier on the eyes (compared to the current red lights). Other advances include improved dissection, a smaller punch (0.8mm), an automatic scar detector, a 20% increase in harvesting speed, the ability for physicians to harvest at an angle as low as 30 degrees from the scalp, and several advances that will make site creation more user-friendly.